System Transformation
- Home: System Transformation
- Foundational Responsibilities and Framework
- Joint Leadership Team
- Innovation Projects (Minn. Infrastructure Fund)
- Governance Groups and Communities of Practice
- Tribal Capacity and Infrastructure
- Local Public Health
- FPHR Grant: Funding for Foundational Responsibilities
- FAQ: Frequently Asked Questions
- Newsletters, Reports, Resources
- Reports, Fact Sheets, Resources
- Newsletter
- Message Toolkit
- Return to Center for Public Health Practice Home
Contact Info

Frequently Asked Questions
Transforming the public health system in Minnesota
Send a question to the Joint Leadership Team online: Ask a Question: Transforming the Public Health System in Minnesota. As the Joint Leadership Team receives questions, it will post commonly-asked questions and answers here and share answers in its newsletter.
- What is the Joint Leadership Team?
- What are foundational public health responsibilities?
- What do foundational responsibilities look like in practice?
- What does "seamless" mean in "a seamless, responsive, and publicly-supported public health system"?
- What does "responsive" mean in "a seamless, responsive, and publicly-supported public health system"?
- Grant and funding: Where can I learn more about funding for foundational responsibilities and the Foundational Public Health Responsibilities Grant?
What is the Joint Leadership Team?
The Joint Leadership Team envisions a seamless, responsive, publicly-supported public health system that works closely with the community to ensure healthy, safe, and vibrant communities. This system of state, local, and tribal health departments will help Minnesotans be healthy regardless of where they live.
This work of strengthening, updating, and transforming the public health system is not led by one single organization. Our inter-governmental relationships are key to making the public health system work. Three groups in Minnesota work together collaboratively, sharing leadership to guide the work of transforming the state’s public health system.
This Joint Leadership Team consists of people from SCHSAC (State Community Health Services Advisory Committee), LPHA (Local Public Health Association of Minnesota), and MDH (Minnesota Department of Health). All three groups are represented at every meeting; the team has met twice per month since 2022 and meetings are led by an independent facilitator.
Outside of meetings, workgroups made up of public health partners (sometimes along with contractors), assess, explore, plan, and execute, laying the tracks for what system transformation means in practice. In parallel, tribal nations we share geography with also consider how to strengthen their own public health infrastructure, as sovereign nations with their own authority, and we continue to communicate and learn from each other.
To learn more and view current Joint Leadership Team members, visit: Joint Leadership Team and Subgroups.
What are foundational public health responsibilities?
Where you live should not determine your level of public health protection. All Minnesotans should have access to comprehensive, high-quality public health, but our system is well-resourced in some programs, topics, and communities, and less so in others.
The foundational responsibilities (below) consist of the population-level activities unique to governmental public health. The responsibilities are divided into five topic areas and eight capabilities, all encircled by equity. These responsibilities should be in place everywhere for public health to work anywhere in Minnesota.
Framework of foundational public health responsibilities
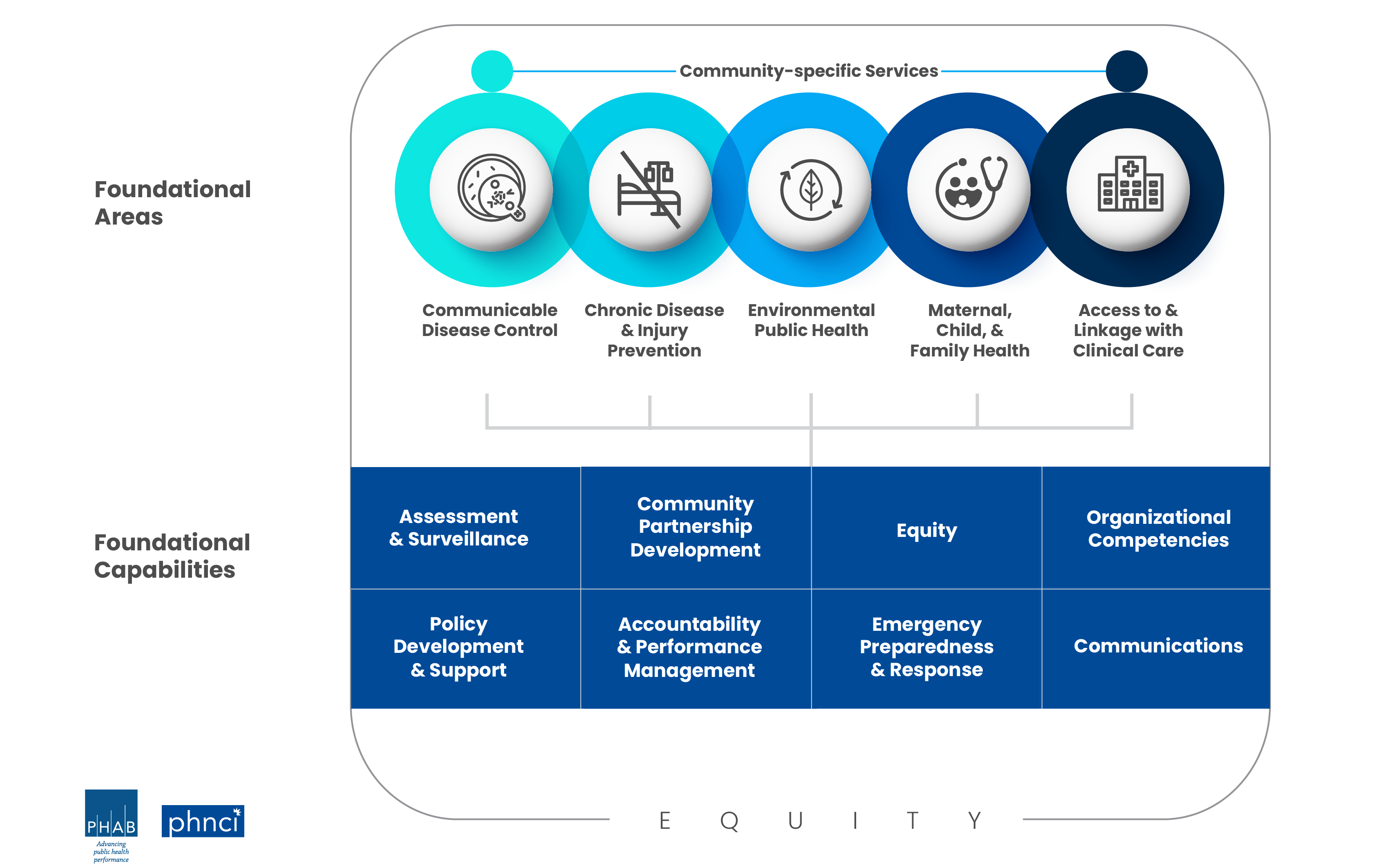
How these responsibilities are carried out will look different depending on local context. Health departments will also provide additional services beyond the foundational responsibilities, as they always have, and may require more or less capacity in different areas and capabilities to best serve their communities.
The whole governmental public health system in Minnesota has a collective responsibility to Minnesotans’ health, and working together to meet foundational responsibilities can equip the statewide system for collective success.
To learn more and see what activities are included in Minnesota, visit: Foundational Public Health Responsibilities and Framework.
What do foundational responsibilities look like in practice?
Public health partners across Minnesota, at the state, local, tribal, and community level, are working together to answer: What would it look like for Minnesota to fulfill the foundational public health responsibilities?
As of April 2024, here are some of the ways we’re finding answers, together:
- Local public health leaders and staff have started to meet each month in a Foundational Public Health Responsibilities Community of Practice, to learn about, discuss, and resolve questions related to foundational areas, capabilities, and how they all fit together in real life.
- MDH and local public health agencies are using data from the 2022 system “cost and capacity assessment” to consider opportunities and challenges for doing foundational work locally and regionally, as discussed in this webinar and Q&A recorded earlier this month.
- To fulfill foundational responsibilities across the system, accountability and transparency are grounded in clear goals and measurement: The SCHSAC Performance Measurement Workgroup is considering how to measure the entire system’s performance by looking at data, monitoring progress, and reporting on trends that indicate opportunities for improvement. The brand new SCHSAC Foundational Public Health Responsibilities Workgroup will recruit members and begin meeting later this spring, to help the system determine the minimum standards for full implementation, locally and system-wide.
- Ongoing, annual funding for foundational public health responsibilities, a down payment on the health of Minnesotans, is supporting local and tribal public health agencies in work related to foundational areas and capabilities.
- Longstanding groups continue to address specific foundational responsibilities, like the Environmental Health Continuous Improvement Board, the Public Health Emergency Preparedness Oversight Group, and the Infectious Disease Continuous Improvement Board (IDCIB)—for example, the IDCIB is aligning Minnesota’s Disease Prevention and Control Common Activities Framework with foundational responsibilities, to ensure Minnesota’s public health professionals consistently and cohesively look for, detect, and prevent infectious diseases.
- Work to strengthen tribal public health moves in parallel to state and local activities: As sovereign nations with their own public health authority, many of the tribal nations Minnesota shares geography with are also assessing their public health infrastructure against national standards, and considering what it looks like to strengthen their work and build capacity to meet their needs.
- The Minnesota Infrastructure Fund is supporting a second round of locally-led, two-year innovation projects, testing new ways of doing foundational public health work that could be used across the state—locally, regionally, or statewide.
- Staff from the MDH Center for Public Health Practice continue to provide convening, connecting, coaching, and technical assistance on foundational responsibilities.
What does "seamless" mean in "a seamless, responsive, and publicly-supported public health system"?
We envision a seamless, responsive, publicly-supported public health system that works closely with the community to ensure healthy, safe, and vibrant communities. This system of state, local, and tribal health departments will help Minnesotans be healthy regardless of where they live. – Joint Leadership Team vision
When we dig into the Joint Leadership Team vision above, what do "seamless," "responsive," and "publicly-supported" mean? What might they look like in a transformed and strengthened governmental public health system in Minnesota?
A seamless public health system works cohesively: across jurisdictions, levels of government, geographies, sectors, and more. Where you live shouldn’t determine your level of public health protection, and every agency that helps shape opportunities for population health can work together to do so. People, diseases, air, water, and soil aren’t bound within jurisdictions—neither is public health.
What would this mean?
- "Everyone’s on the same page—we’re not talking past each other."
- "We have clear roles and responsibilities for who does what, and mechanisms to coordinate, communicate, and maintain partnerships."
- "We’re highly collaborative."
- "I’m not feeling alone out in the ‘public health woods.’"
- "It’s easier for partners to work together—the rules for public health don’t change when we cross jurisdictional boundaries."
What might this look like?
- “Hub” service models, like a one-stop shop for food inspection so customers don’t have to interface with many entities.
- Standardized ways of sharing data across public health partners; data flows easily through the system and partners can use it to inform decisions.
- Strong local relationships between government and community, so partners don’t have to “leapfrog” their localities to find someone they know or trust.
What does "responsive" mean in "a seamless, responsive, and publicly-supported public health system"?
We envision a seamless, responsive, publicly-supported public health system that works closely with the community to ensure healthy, safe, and vibrant communities. This system of state, local, and tribal health departments will help Minnesotans be healthy regardless of where they live. – Joint Leadership Team vision
When we dig into the Joint Leadership Team vision above, what do "seamless," "responsive," and "publicly-supported" mean? What might they look like in a transformed and strengthened governmental public health system in Minnesota?
We envision a public health system that can react quickly and effectively to today’s opportunities and challenges, plan for tomorrow’s, and use lessons learned from the past to grow stronger and more capable.
What could this mean?
- "We can address root causes, not just fill immediate gaps."
- "We can quickly adapt and adjust to emerging threats, challenges, opportunities."
- "We can meet community needs, especially where there are disparities."
- "We can trust each other’s capacity to partner on work."
- "We can work upstream to address the structural and social drivers of health."
What might this look like?
- Quick and timely data to respond to emerging threats, especially locally
- An agile workforce that can respond to changes, is well-trained, and can see a consistent pathway into public health careers
- A public health workforce that reflects the community it serves
Where can I learn more about funding for foundational responsibilities and the Foundational Public Health Responsibilities Grant?
For more logistics- and operations-oriented questions about foundational public health responsibility funding, grant requirements, invoicing, and more, please visit Funding for Foundational Public Health Responsibilities and scroll to "frequently asked questions."